Due to the pandemic causing various complex situations, which are unpredictable, we can only rely on adaptability, but the principles remain unchanged.On May 25, 2022, the shipowner association’s agent sought assistance: there is a Chinese crew member with severe schizophrenia who has been treated in a psychiatric hospital in Rio de Janeiro, Brazil, for over a month. Local doctors believe he can return to China with professional accompaniment.Medical transport during the pandemic has many uncertainties:
- Airfare is exorbitantly high, and obtaining a green health code may be impossible (for various reasons), leading to forced repatriation.
- There is a risk of contracting COVID-19 en route.
- Layovers may result in being denied boarding, with the possibility of being quarantined on-site.
- There could be awkward situations where entry is impossible, and return is also not feasible, leading to potential delays of several months.
Brazil is a high-risk country, with no control measures in place and a population achieving herd immunity.However, the shipowner association is very determined to rescue this crew member, believing that expenses can be managed compared to the value of life. Under these circumstances, “Anhe Aid” contacted the airline through a first-class ticket agent to arrange internal ticketing, with one ticket costing nearly 100,000 RMB.The accompanying doctor arrived in Rio de Janeiro and assessed the patient, finding the situation still manageable. Thus, they entered a monitoring period (as stipulated by the Chinese embassy, all returnees from Brazil must stay for 10 days before applying for a green health code). However, on the third day, the accompanying doctor began to have a fever and tested positive for COVID-19, making a diagnosis almost certain.Crisis management steps:
- Treat the illness: Ensuring the accompanying doctor recovers (whether this falls under professional liability insurance is still uncertain, especially since it was not confirmed that the patient infected the doctor, but the recovery of the accompanying doctor is a principle).
- Monitor ticket changes: Closely track the costs of rebooking and refunds, dates, and ticket insurance (with flights drastically reduced during the pandemic, each step must be taken with caution to avoid significant losses).
- Stabilize the patient’s emotions: Communicate with all parties and coordinate opinions.
The call center plays a crucial role in crisis management.
Consultations with domestic and American experts on the best treatment plans for COVID-19 were conducted to select the most suitable communication with local doctors. Local agents were asked to provide necessary services: delivering medicine, food, and other daily necessities, scheduling check-ups, tests, and consultations.
Daily updates on the local doctor’s situation were recorded, feedback was prepared, emotions were soothed, and recovery was promoted.
Every decision regarding ticket refunds and rebookings required contacting the shipowner association for approval before execution.
Close attention was paid to policy changes, maintaining good interaction with the embassy.
After about two weeks of active treatment, the local doctor nearly recovered, at which point he visited the patient for a final assessment. However, the patient’s condition relapsed, showing severe manic tendencies.
After about two weeks of active treatment, the local doctor nearly recovered, at which point he visited the patient for a final assessment. However, the patient’s condition relapsed, showing severe manic tendencies.
Crisis management was reactivated:
With the shipowner association’s consent, the ticket was rebooked (pandemic behavior must adhere to the highest principle: safety during transit).
The local doctor continued to rest, ensuring proper nutrition and moderate exercise for a swift recovery.
The patient’s attending physician was asked to change the medication, ensuring the condition remained manageable for the journey home.
On July 10, all aspects aligned, meeting the embassy’s requirements, including ticket timing and conditions for a return via Amsterdam.
On July 11, the layover in Amsterdam required a COVID-19 test the next day. Hotels at the airport were fully booked, and sleeping on terminal benches was the only option. However, on July 12, the patient’s test result was positive, prohibiting further travel and necessitating local quarantine, while the doctor’s test was borderline, allowing travel.
Crisis management was initiated again:
After weighing the pros and cons of several options, the final decision was made: abandon quarantine in Amsterdam and choose a stay in Bangkok, which offered relatively reasonable living standards and medical conditions more suited to Eastern lifestyles (other countries had more relaxed policies, which also posed a risk of infection on the flight).
The ticket was changed to fly to Bangkok for a stay until a negative test was obtained.
On July 16, they arrived at a hotel in Bangkok to rest, conducting daily COVID-19 tests to meet embassy requirements. Simultaneously, attention was given to the isolation between the doctor and patient, providing the patient with appropriate COVID-19 treatment. After fulfilling all conditions, they checked into a quarantine hotel before departure on July 25. Everything proceeded smoothly; the first round of tests was negative, and the second round was also negative, preparing to apply for the green health code. The patient received a red health code and was denied, with the reason being non-compliance with the required quarantine period. However, the accompanying doctor could return home.
Crisis management was initiated for the fourth time:
Due to the lengthy journey, the doctor’s health was also a consideration, leading to the decision for the doctor to return home first.
Thai agent services were activated: a Thai-Chinese agent assisted the patient in checking into an apartment for self-isolation for two weeks, with the doctor remotely managing the patient’s medication (psychiatric drugs).
During the long month, the patient developed significant trust in the accompanying doctor, fully complying with their instructions, leading to noticeable control of the condition. After the accompanying doctor had to return home, remote management continued to soothe the patient’s emotions and correct their behavior.
The call center monitored the patient’s daily diet and medication adherence through WeChat.
Unexpected situations arose again. Thailand maintained an open stance on asymptomatic COVID-19 cases. The “Anhe Aid” call center arranged for the patient to visit a local international hospital’s psychiatric department for medication after scheduling an outpatient appointment.
The patient exhibited emotional fluctuations, smoking over ten cigarettes daily and frequently seeking smoking areas.
Throughout this round of isolation, the tests remained negative, but on the final day, the test was positive, prompting the hotel and airline to notify the embassy.
The embassy’s mandated quarantine schedule was repeated. During this period, the “Anhe Aid” call center maintained close communication with the Bangkok agent, guiding them to contact the embassy, liaise with Thailand’s foreign affairs department for visa extensions, and arrange for the patient to go out for haircuts, shopping, and psychiatric follow-ups for medication.
Monitoring of the agent’s and patient’s progress, along with daily diet and medication tracking, continued. Remote patient reassurance efforts persisted, with the already returned accompanying doctor maintaining contact with the patient, continuously checking in on their condition, coordinating with the agent to enhance the patient’s nutrition, ensuring relatively independent meals, correcting bad habits, and teaching them to continue nasal rinsing. Finally, on September 6, all COVID-19 tests were negative, and the green health code was approved, allowing for the return home.
Final Verdict
From June 9, when medical transport services were initiated, to the actual conclusion on September 17, when the patient returned home, this case spanned over three months, marking the longest medical transport case in history.
The key to successfully completing this case lies in:
- Balancing various factors: Under the premise that the patient must return home with an accompanying person, make choices that minimize costs and are the most humane decisions.
- Leveraging Chinese resources in different locations: Providing timely assistance and support is crucial, enabling the highest quality and cost-effectiveness of services.
- Excelling in remote services: Through WeChat communication, the full potential of remote services can be realized.


COVID-19 Testing Negative on Aug.9, while Positive on Aug. 10
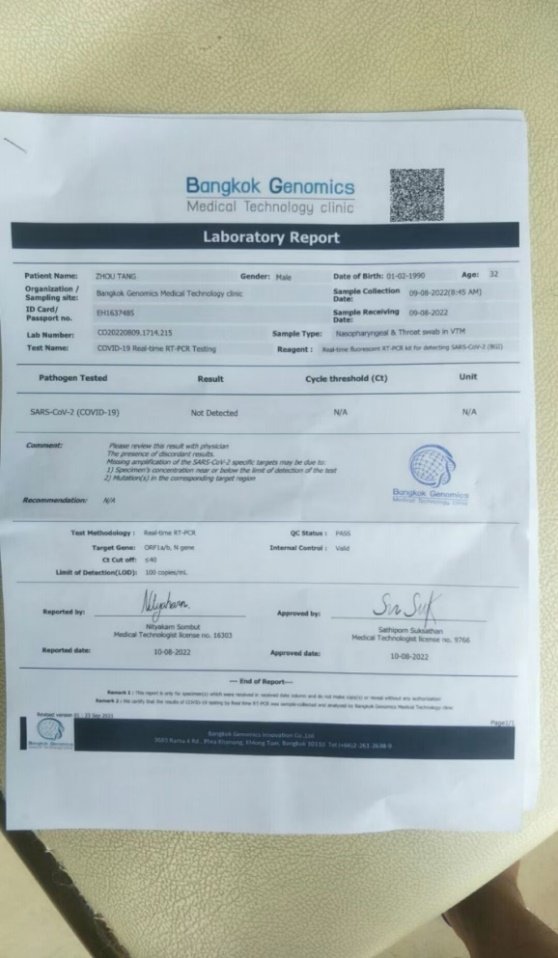
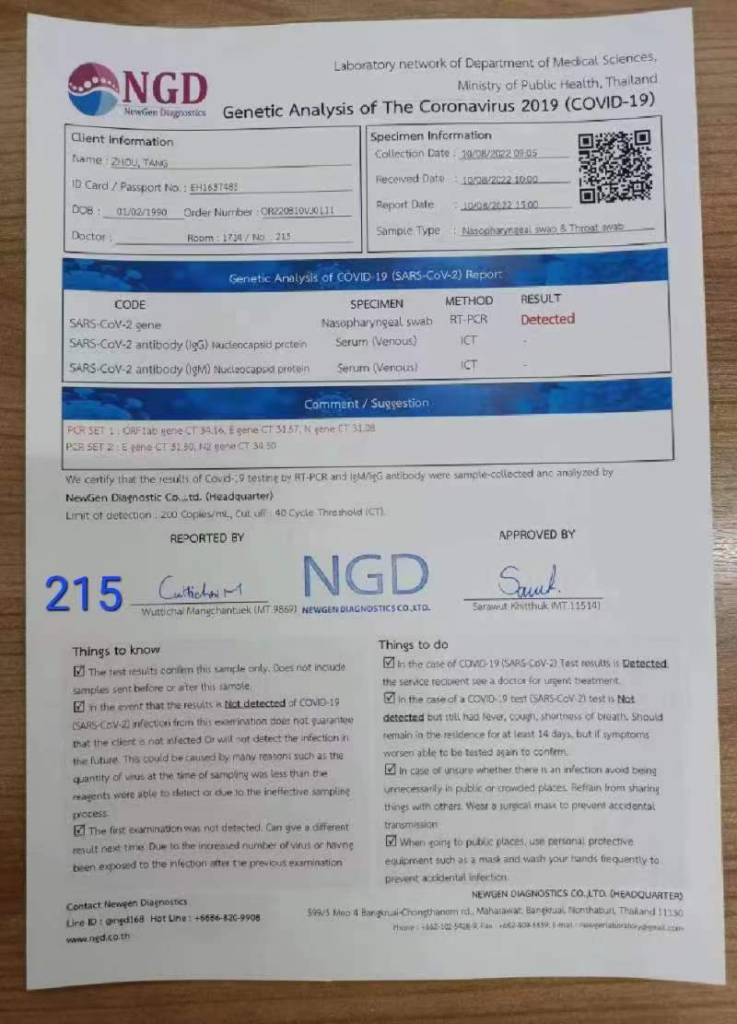
the patient and the doctor completed the COVID-19 test in Brazil as a keepsake





.pdf-image-009.jpg)
.pdf-image-010.jpg)
